|
News Detail
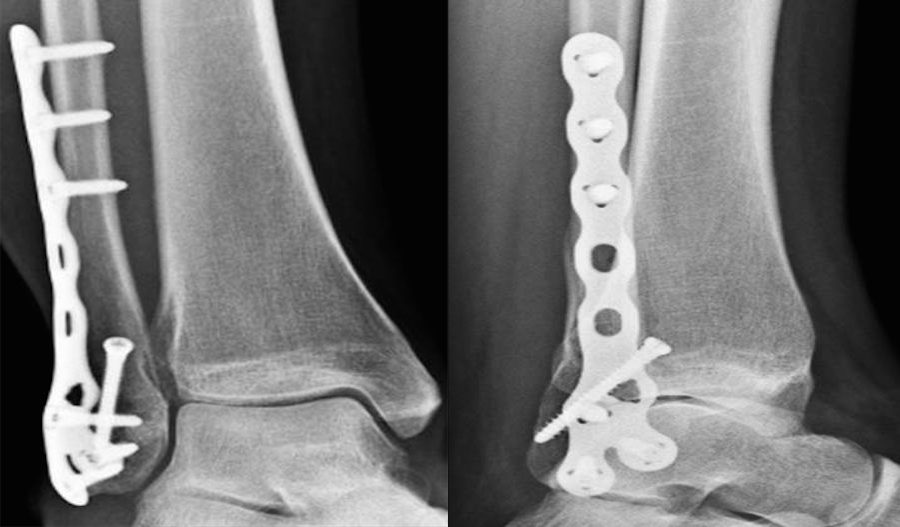
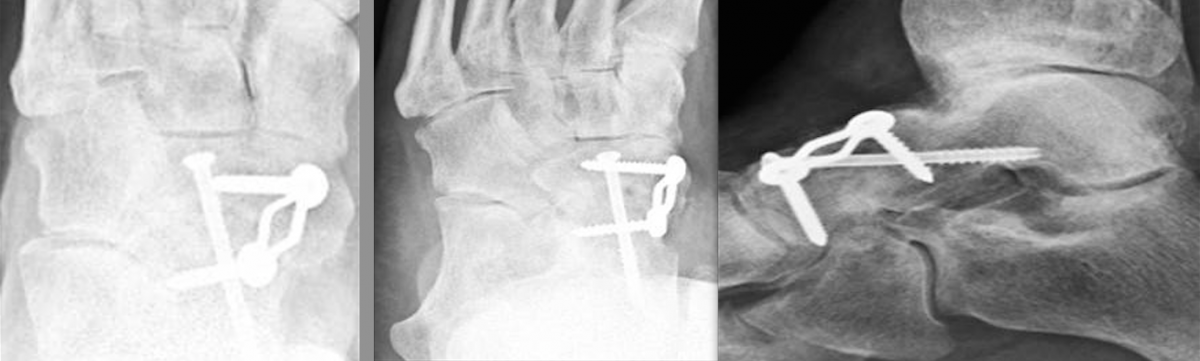
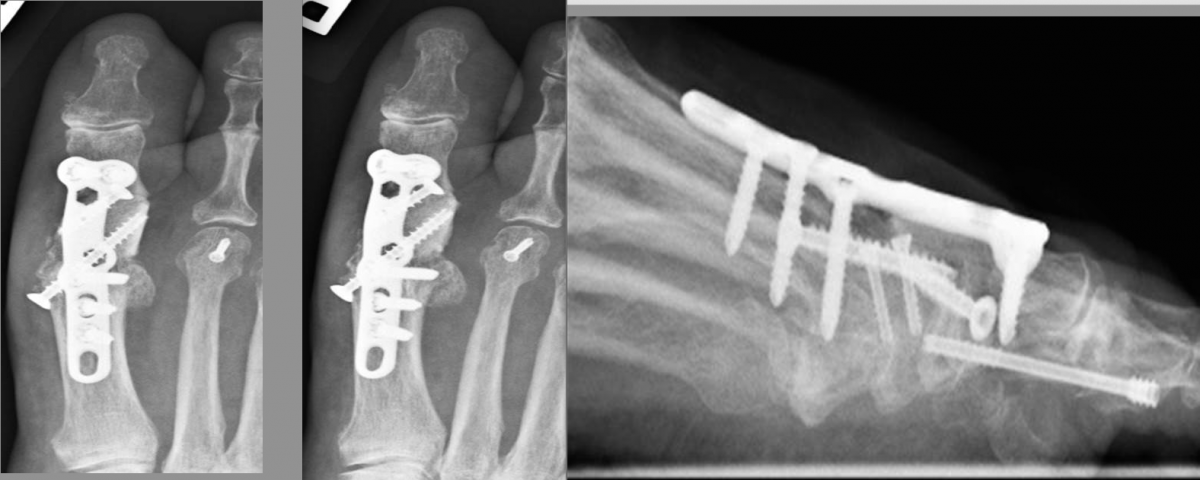
Locking Plates: What Have We Learned? Although traditional plate designs date back decades, these authors discuss the emergence and potential of locking compression plates, polyaxial locking plates, and minimally invasive plate osteosynthesis. HYPERLINK "https://s3.amazonaws.com/HMP/hmp_ln/imported/pt0915locking1ab.png" \t "_blank" The popularization of traditional plate and screw constructs dates back to the late 19th century as well as the efforts of the Belgian surgeon Robert Danis, MD.1,2 This discovery along with Danis’ publication of Over the past several decades, as surgeons have gained a better understanding of the utility of plate and screw constructs, the application of the devices has evolved. In addition to incorporating these devices into the surgical repair of fractures, surgeons may utilize them for joint arthrodesis and other reconstructive osseous surgeries. One advance with these modalities has been the advent and evolution of the locking plate construct, which has several applications within foot and ankle surgery. Reviewing The Different Kinds Of Plate Fixation HYPERLINK "https://s3.amazonaws.com/HMP/hmp_ln/imported/pt0915locking1cd.png" \t "_blank" Neutralization plates function as load-sharing apparatuses that shield lag screws from the torsional forces the surgeon encounters during range of motion.4 Buttress plates and anti-glide plates are load-bearing devices that can support a section or segment of bone, which are frequently areas of impaction associated with significant comminution of the cortex, thus leaving a compromised diaphyseal construct and/or voids within the cancellous bone. By fixing the plate proximally and distally to stable areas of bone, the surgeon can prevent the segments from re-approximating during axial loading.5 There are two kinds of compression plates: static compression plates and dynamic compression plates. With the static compression plate, the compression yielded at the fracture interface is secondary to the tension one applies to the implant. This technique is beneficial for those transverse or short oblique fractures when insertion of a lag screw is not attainable. In order to achieve compression, drill the initial screws eccentrically through oval holes in the plate away from the fracture site. As the screw heads contact the plate and sit centrally in the oval holes, the fragments compress together. The dynamic compression plate adheres to the tension band principle. This refers to the application of a plate on the tension (convex) side, preventing gapping that normally would occur and converting the distracting forces into compression forces. The placement of a plate to bone serves as both an expediter and a temporary inhibitor of osseous repair.5 HYPERLINK "https://s3.amazonaws.com/HMP/hmp_ln/imported/pt0915locking2abc.png" \t "_blank" Certain plate designs have addressed the effects of reduced blood flow that can occur underneath a plate due to reduced bone density. This plate-associated osteoporosis has a detrimental effect on the mechanical properties of healing bone. Limited contact dynamic compression plates were designed with recesses or undercuts in the plate to reduce contact between the plate and the bone, therefore reducing the risk of plate-associated osteoporosis. Recognizing The Potential Benefits Of Locking Compression Plates There have been efforts to improve the weakest part of the construct (the screw-bone interface) by increasing the contact area between the screw and the bone with the placement of screws in polymethyl methacrylate (PMMA) or by creating a single-beam construct. This is the principle behind locking plates with the creation of a construct to address the lack of motion between the components of the beam (i.e., the plate, screw and bone).6 HYPERLINK "https://s3.amazonaws.com/HMP/hmp_ln/imported/pt0915locking2def.png" \t "_blank" The locking compression plate arose from the desire to increase stability, which at the time was limited by the torque generated during screw purchase into the plate-bone interface. Cancellous, osteoporotic or pathologic bone and comminution limit the amount of torque that one can generate to enhance stability.7 This led to the development of the locking compression plate, which has the ability to preserve the blood supply to bone by reducing periosteal stripping. The traditional plating techniques provided stability by compressing the plate to the bone surface with the screws achieving bicortical purchase as the second point of fixation. However, locking compression plate technology features unicortical locking screws that can be an “internal fixator” that can act as a bridge over compromised bone.8 However, in areas or regions where high torsional and axial loads are expected, one should utilize bicortical locking screws. With locking plates, the sum of all the interfaces between the screws and bone equals the strength of fixation as opposed to the unlocked plates’ single screw pullout strength.7 One of the benefits of locking plates is their ability to be “bridge plates,” whereby they provide excellent axial and angular stability, preserve fragmentary blood supply, and reduce the risk of loss of reduction. Indeed, surgeons do not have to contour these plates anatomically to the bone, and the plates have the potential benefit of providing superior fixation in osteoporotic bone. Indications for the use of locking plates include diaphyseal/metaphyseal fractures in osteoporotic bone, multifragmentary diaphyseal/metaphyseal fractures, osteotomies in at-risk patients (poor bone stock, revisions, etc.), articular fractures, segmental fractures with multiple patterns, and any combination of the above.9 HYPERLINK "https://s3.amazonaws.com/HMP/hmp_ln/imported/pt0915locking3ab.png" \t "_blank" In their guidelines for using the locking compression plate, Gautier and Sommer emphasize the importance of the reduction technique, minimally invasive plate insertion and fixation to keep bone viability undisturbed.9 Pertinent Insights On Minimally Invasive Plate Osteosynthesis HYPERLINK "https://s3.amazonaws.com/HMP/hmp_ln/imported/pt0915locking3cd.png" \t "_blank" Minimally invasive plate osteosynthesis maintains bone vascularization with minimal periosteal stripping, thus improving bony consolidation and decreasing operative time, complications and infection rates. The application of a locking plate using the minimally invasive plate osteosynthesis technique generally consists of making small incisions proximal and/or distal to the fracture site, percutaneous reduction and subsequent extraperiosteal placement of the plate with any radiolucent percutaneous guide. Can Polyaxial Locking Plates Have An Impact? A recent study by Cullen and colleagues looked at a biomechanical comparison of polyaxial and uniaxial locking plate fixation in extra-articular proximal tibia metaphyseal fractures.10 A Closer Look At Potential Contraindications And Complications Currently, there are no absolute contraindications for locking plates. However, there are instances when applying them may be unnecessary. A good example would be in a case with a simple fracture pattern in a healthy patient with good quality bone. Another case would be a fracture pattern where the surgeon is trying to achieve compression through the plate itself without the addition of a lag screw. Also, if a patient has an oligotrophic non-union and the cause of the delayed healing is not related to an insufficient amount of stability, one should not employ locking plates. Another matter to keep in mind is the increased cost of a locking plate-screw construct versus traditional plate-screw designs, which in some cases can be substantial. As always, consider the possibility of a metal allergy or intolerance. HYPERLINK "https://s3.amazonaws.com/HMP/hmp_ln/imported/pt0915locking4def.png" \t "_blank" One of the more common complications with locking plates is creating an environment of too much stability, thus becoming “non-union generators.”11 Final Thoughts As we previously discussed, it is important to tailor the fixation of choice to the fracture pattern and location, the underlying bone quality and the overall needs of the patient. We still need to see more clinical data on locking plate technology in order to determine specific clinical scenarios in which the additional cost may be justified. Dr. Fidler is a Fellow at the Orthopedic Foot and Ankle Center in Westerville, Ohio. Dr. Prissel is a Fellow at the Orthopedic Foot and Ankle Center in Westerville, Ohio. Dr. Hyer is the Fellowship Director of the Advanced Foot & Ankle Surgical Fellowship in Westerville, Ohio. He is a Fellow and a member of the Board of Directors for the American College of Foot and Ankle Surgeons. References 1 2 3 4 5 6 7 8 9 10 11
|